Automating Prior Authorization at the Point of Care
For healthcare providers, prior authorization (PA) via fax or telephone is the second most costly medical administrative function. On average, medical staff spend two business days per week on PA. Automating PA while maintaining clinical excellence is essential for better care delivery. With a focus on leveraging digital solutions and fostering data-enabled decisions, Magellan Healthcare is building more provider-friendly approaches to improve care.
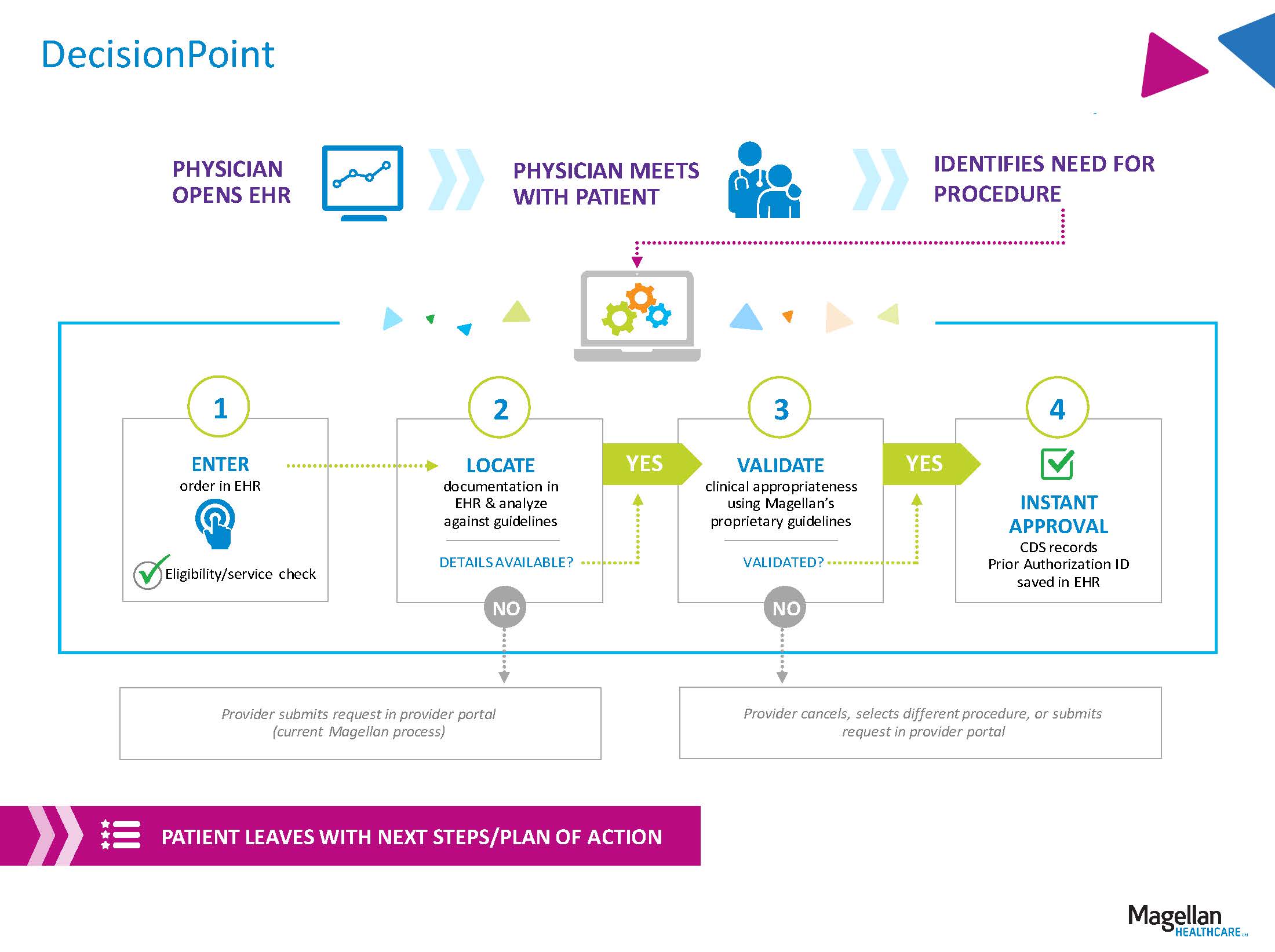
Recently Magellan announced a collaboration with Stanson Health, Premier, Inc.’s clinical decision support (CDS) technology division, to deploy DecisionPoint, an industry-leading automated PA solution. Powered by Premier’s CDS technology, DecisionPoint is available at the point of care and supports true automation within the electronic health record (EHR) and the physician workflow, making the PA process easier and more efficient for providers, patients and health plans.
DecisionPoint is built with Magellan Healthcare’s Advanced Imaging Management program clinical guidelines and Premier’s award-winning technology platform. Magellan maintains one of the industry’s most comprehensive evidence-based sets of clinical guidelines. Our clinicians develop our criteria through an extensive process of innovation and refinement. We base these guidelines on the analysis of public, peer-reviewed articles; health plan medical policies; the Centers for Medicare & Medicaid Services (CMS) policies; specialty physician reviews, professional society guideline statements; and other rigorous reviews of scientific documents. We continually monitor peer-reviewed literature, professional society guideline statements, and CMS-covered criteria to update our guidelines regularly, no less than annually. Initially, DecisionPoint will include our suite of the 20 highest-volume advanced imaging studies that make up 85% of all requests.
Working directly in the EHR, DecisionPoint guides provider decisions in real time in response to key workflow events, such as ordering an advanced imaging study. Integrating within the EHR improves efficiency while ensuring safety and quality and reducing undesirable variation in care.
Rules-based programming leverages EHR data, locating all relevant patient clinical information and citing appropriate Magellan clinical guidelines. Requests that satisfy the clinical guidelines are automatically approved and posted in the EHR, and approval IDs are automatically loaded to the record. With a confirmed authorization determination, the member leaves the appointment with a clear plan of action.
Hawai‘i Pacific Health (HPH), one of the largest healthcare providers in Hawai‘i, is leading the way in automating prior authorization by piloting DecisionPoint to help ensure their patients receive real-time, evidence-based decisions at the point of care whenever possible. Administered through HPH’s Accountable Care Organization (ACO) with over 800 physician members, the pilot leverages Magellan’s clinical guidelines and our full panel of clinical experts. We expect DecisionPoint to be available to additional providers in the fourth quarter of 2019 and include additional specialties and tests in the future.
The healthcare industry is in the midst of a significant paradigm shift as it transitions from a fee-for service model to value-based care. As a technology-augmented service backed by the support of providers, DecisionPoint is designed to minimize the industry’s challenges by fully integrating with EHRs at the point of care to enable faster PA and help deliver on the triple aim—improved quality, reduced cost and improved patient/provider experience.
To learn more about DecisionPoint, click here to go to our website, or email ProviderSolutions@MagellanHealth.com.