Many of us can now say we have experienced the trials and tribulations of parenting during a pandemic. We have attempted to juggle full-time work and regular household duties, along with being a full-time teacher or daycare worker and entertainer for our kids. While we’re all doing the best we can in taking on these new and challenging roles, some parents and caregivers may be wondering about their child’s mental health after they have missed out on so much and dealt with new stress and uncertainty – certainly as many of us know that our own mental health has been affected.
If you’re worried about your child’s mental health or noticing any issues, read on for tips and knowledge shared by Magellan’s Linda Y. Evans, MD, FAPA, child psychiatrist and medical director, and Greg Dicharry, CPRP, youth empowerment director.
Children behavior changes
Changes in your child’s behavior may be a sign of mental health difficulties that should be closely monitored. Depending on the age of your child, stress can manifest in different ways. Toddlers and young children aged 2-6, may show signs of regression and lose the ability to do things previously learned, like toilet training. School-aged children and teenagers may show a disinterest in going to school and/or begin to see falling grades. The most common symptom in teenagers is irritable mood. Kids of all ages may experience vague body complaints, like a headache or belly ache, changes in sleep or appetite, difficulty concentrating, loss of pleasure in activities previously enjoyed, and withdrawal from social interactions.
Often, even the child may not recognize these symptoms as the result of mental health issues. It is important for parents and caregivers to be a barometer for behavioral or other changes in their children – as they may be the first to notice – to be able to identify if their mental health may be suffering. When parents keep the lines of communication open, allowing their kids to share their thoughts and feelings, they are better equipped to identify any troubling signs of childhood depression, anxiety or other mental health conditions.
The child’s primary care physician (PCP) also plays a role in screening for mental health concerns and can be a good first point of contact if parents are seeking additional help. With the shortage of child psychiatrists and mental health professionals trained to work with children in our country, PCPs are increasingly adopting a model of collaborative, or whole-person, care to screen and treat children for mental health issues before they get worse because of potentially waiting long periods to see a specialist.
Interrupted school and family routines
While there’s not much we can do about changing work, school and social arrangements due to the pandemic, it’s important to consider the stability of our kids’ environment and instill predictability in their lives to the extent that’s possible.
Additionally, there are many things that parents and caregivers can do to keep their kids content and engaged amid the chaos and unprecedented change we’re all experiencing. To make up for lost in-person social time with friends and family, virtual meetups can be scheduled. That could be a fifteen-minute Facetime call with grandma and grandpa every Wednesday night at 7:00, or a periodic Zoom/interactive video game gathering with friends. Parents can also take time with their kids away from the screens to play a board game or do a project to make home-time more fun. Exploring and supporting your kids’ passions is a way to get them involved in activities that will bridge the gaps of interrupted routines and help prevent negative mental health outcomes.
Family stress affecting children
We have all been affected by the drastic changes, uncertainty, loss and isolation caused by COVID-19. And it’s not hard for our own stress and worry to be noticed or even absorbed to some extent by our kids. While we’re focusing on our family’s well-being, it’s important to practice self-care and recognize that our own mental health is of paramount importance. Having healthy caregivers is an essential component in the normal development of kids.
When parents are navigating divorce and co-parenting arrangements during COVID-19, it can be even more difficult to filter out the negativity for our kids, especially when parents have different points of view about things like in-person vs. virtual learning, the vaccine and mask wearing. Although it can be difficult to share your kids with an ex-spouse, it’s important to remember they need both of their parents. When parents work together for the benefit of their children and keep the focus on them, the impacts of divorce can be mitigated. Implementing a flexible custody arrangement during COVID-19 is also encouraged; for example, if the child wants to see a parent when it’s not their day for visitation, it might be beneficial to the child to honor their request.
To alleviate stress and some of the burden, parents and caregivers can consider connecting with others who understand the struggles and support each other. They can look for parent support groups in their communities.
Back to school and bullying
For kids who experience any level of social anxiety, the transition back to school, or even a new school, from the comfort of home may be more difficult. While some kids may be happy to get right back to the in-person learning environment, a gradual adjustment may work better for others.
Teachers can be especially helpful in ensuring that children are adjusting well and that a child withdrawing from the group is noticed. When the teacher has a trusting relationship with students, they can initiate conversations to try to understand how a child is doing and if their emotional needs are being met. The teacher’s insights are critical for parents and caregivers who cannot be with their kids at school.
Parents and teachers should be especially sensitive to look for bullying and have a zero-tolerance policy for kids being cruel to one another. Children must understand that bullying is unacceptable, as it can lead to serious and disastrous consequences for those who are targeted.
In general, what kids need for healthy development is a stable routine, predictability, a safe environment and healthy parents or caregivers. COVID-19 has disrupted all of these conditions, leading to increased mental health disorders and interrupted development. There are many things that parents and caregivers can do to nurture their child’s mental health and address what they need for healthy development. We encourage you to explore Magellan’s following resources for additional information and support:
- Mental Health Month website for comprehensive tips and resources to support yours and your family’s mental health.
- Be sure to check out the recording of our webinar, How are your kids doing? under “Previous events”
- Understanding and Meeting the Needs of Children and Adolescents at High Risk: Foundations of a Model clinical monograph highlighting evidence-based research on the prevention and treatment of problematic behaviors and various types of behavioral health challenges in children and adolescents.
- Stay Home for MY LIFE virtual youth fest, featuring inspirational speakers, uplifting entertainment, fun activities and more, taking place on the 4th Thursday of each month, from 6:00 – 7:30 p.m. ET, for youth and young adults who have experience with mental health, substance use, juvenile justice and foster-care-related issues, as well as professionals and caregivers across the country.
 Jamie Hanna, MD, serves as the medical director for the Magellan of Louisiana Coordinated System of Care (CSoC) program. She is board certified in Psychiatry and Child and Adolescent Psychiatry. Prior to joining Magellan in 2020, Dr. Hanna served as an assistant professor and assistant training director with Louisiana State University School of Medicine, working with the acute behavioral health unit, and leading the psychiatric consultation-liaison service and emergency psychiatric services at Children’s Hospital of New Orleans. Dr. Hanna completed medical school at the University of Alabama School of Medicine and a subsequent internship in Pediatrics, residency in General Psychiatry, fellowship in Child and Adolescent psychiatry, and fellowship in Infant Mental Health with Louisiana State University in New Orleans.
Jamie Hanna, MD, serves as the medical director for the Magellan of Louisiana Coordinated System of Care (CSoC) program. She is board certified in Psychiatry and Child and Adolescent Psychiatry. Prior to joining Magellan in 2020, Dr. Hanna served as an assistant professor and assistant training director with Louisiana State University School of Medicine, working with the acute behavioral health unit, and leading the psychiatric consultation-liaison service and emergency psychiatric services at Children’s Hospital of New Orleans. Dr. Hanna completed medical school at the University of Alabama School of Medicine and a subsequent internship in Pediatrics, residency in General Psychiatry, fellowship in Child and Adolescent psychiatry, and fellowship in Infant Mental Health with Louisiana State University in New Orleans. Dr. Tonicia Freeman-Foster has over 20 years of experience in cultivating hope, resiliency, and wellness through her work with underserved persons and marginalized communities. She is passionate about her work in assisting organizations and leaders in understanding how their beliefs and actions impact diversity, equity, inclusion, belonging, and justice for staff, clients, and communities. Dr. Freeman-Foster possesses extensive experience in matters related to mental health, substance use, child welfare, HIV/AIDS, and LGBTQ+, youth and young adult, women, Black, Indigenous, and People of color (BIPOC) populations.
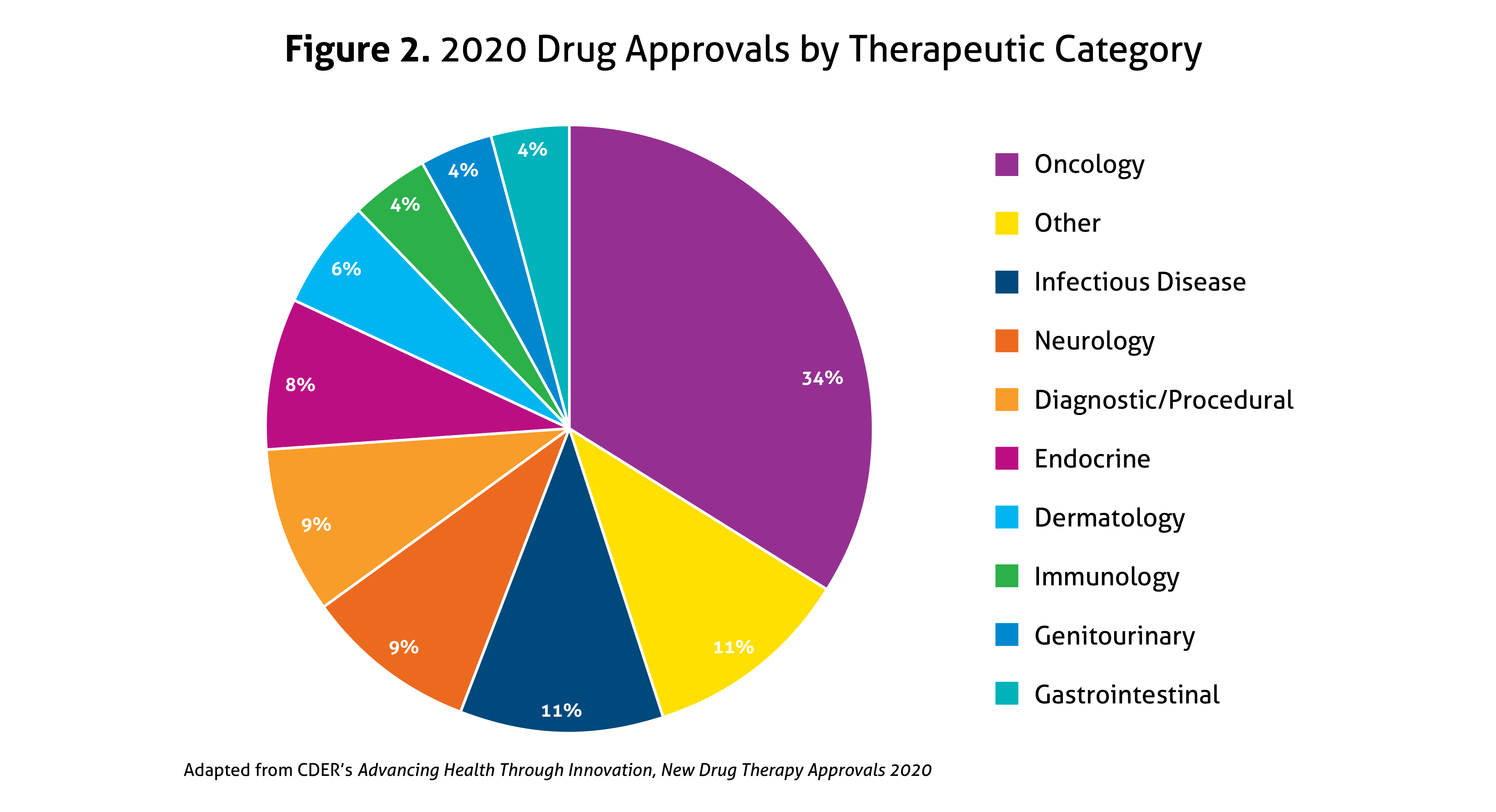
Dr. Tonicia Freeman-Foster has over 20 years of experience in cultivating hope, resiliency, and wellness through her work with underserved persons and marginalized communities. She is passionate about her work in assisting organizations and leaders in understanding how their beliefs and actions impact diversity, equity, inclusion, belonging, and justice for staff, clients, and communities. Dr. Freeman-Foster possesses extensive experience in matters related to mental health, substance use, child welfare, HIV/AIDS, and LGBTQ+, youth and young adult, women, Black, Indigenous, and People of color (BIPOC) populations. 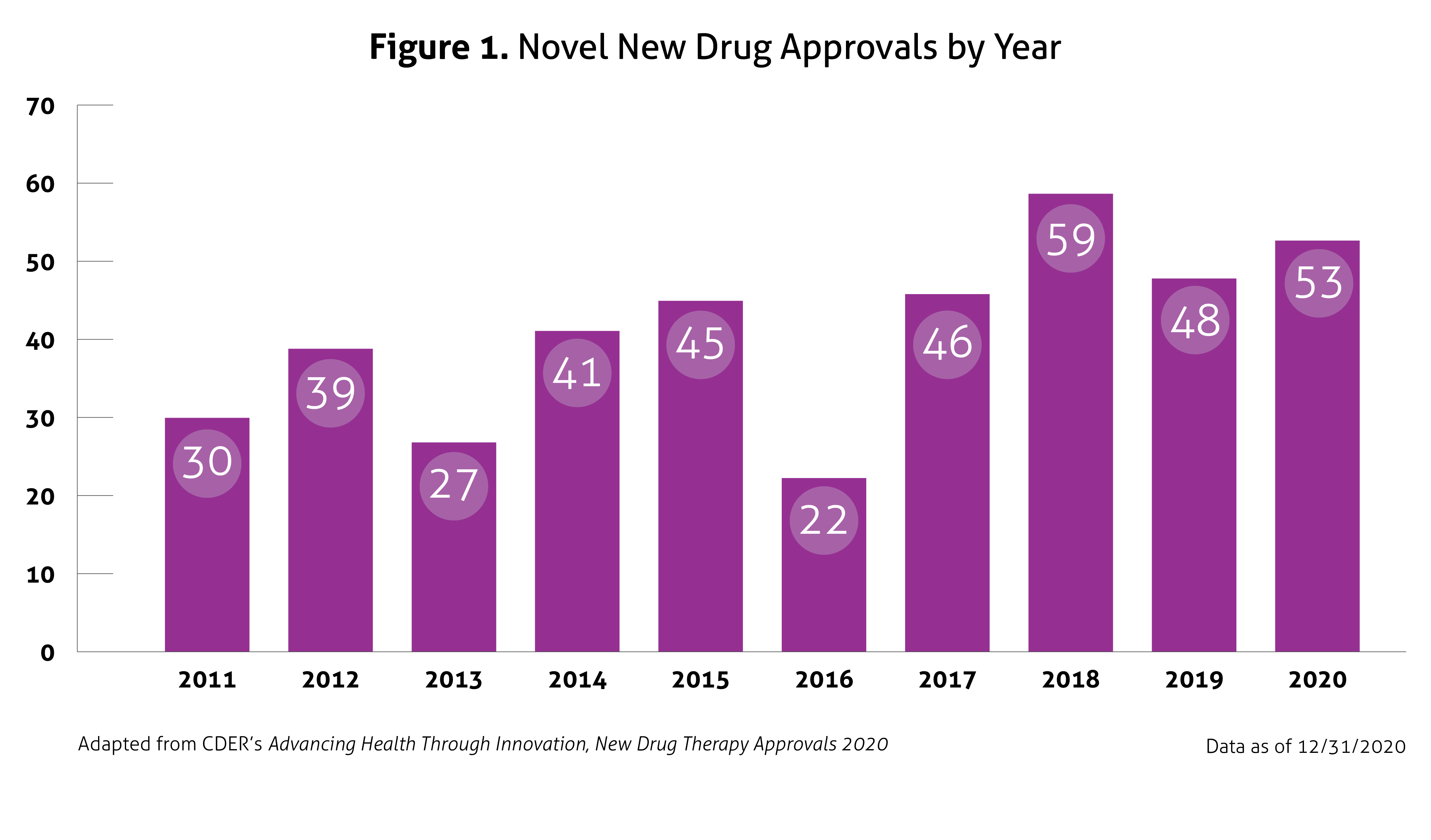 Despite the ongoing pandemic the FDA continued their strategic initiatives to expedite the safe review of treatments in 2020. With the unprecedented challenges incurred in 2020, the FDA acknowledged that maintaining their commitment to bringing forth innovative therapies was difficult. Remarkably, the numbers reported by the FDA do not include the several emergency use authorizations (EUAs) issued by the FDA for COVID-19.
Despite the ongoing pandemic the FDA continued their strategic initiatives to expedite the safe review of treatments in 2020. With the unprecedented challenges incurred in 2020, the FDA acknowledged that maintaining their commitment to bringing forth innovative therapies was difficult. Remarkably, the numbers reported by the FDA do not include the several emergency use authorizations (EUAs) issued by the FDA for COVID-19.